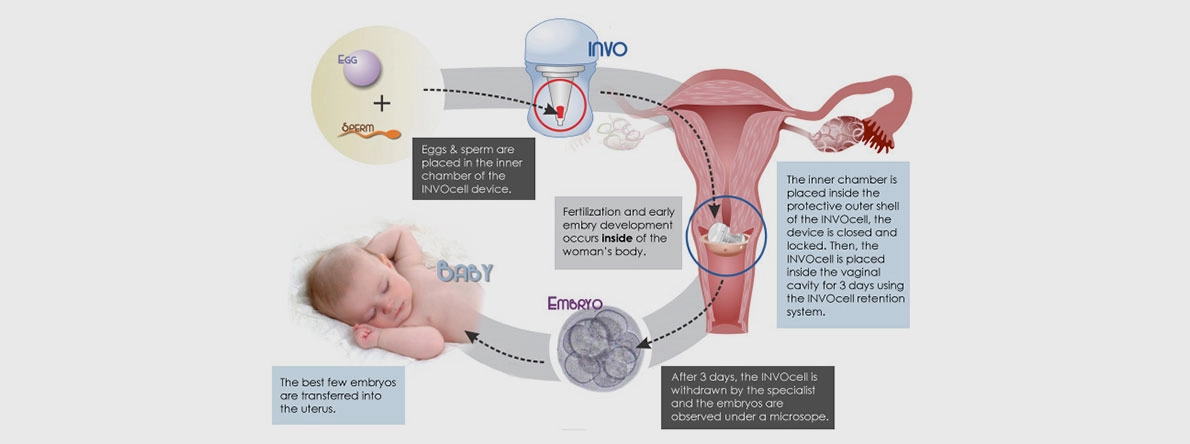
INVOcell is a vaginal device marketed as a low-cost incubator for eggs and sperm after eggs are retrieved following IVF with mild ovarian stimulation using fertility drugs.
Ovaries are motivated with 150-225 units of stimulating drugs. Up to 10 oocytes are inserted in the INVOcell capsule which is placed high in the vaginal cavity for 3-5 days. At that time, the embryos are examined once and the 1-2 best embryos are transferred to the uterus. While INVOcell does have advantages, there are significant drawbacks compared to regular IVF in addition to not being cost-effective compared to mini-IVF; here are some examples.
- With INVOcell, the culture medium is not changed for 5 days. It is beneficial for a culture medium to be changed on D3 of life when embryos grow from 8 cells on day 3 to 120 cells on day 5 of life. For this reason, blastocyst media are different from day 3 media. Changing the medium more frequently also lowers the risk of infection, since any infection would cause the loss of all the embryos. The future survival of those embryos when frozen, after being cultured with this method, is still uncertain.
- “Effortless”. Many may find it nerve-wracking to carry embryos for 5 days in their vaginal cavity instead of the safety of a doctor’s IVF Laboratory.
- Embryos are not checked after fertilization. This means that if more than one sperm fertilized an egg (polyspermy) or if eggs had extra numbers of maternal chromosomes (polygyny), these chromosomal abnormalities would be missed. Whether the risk of trophoblastic tumors is increased as a result of this hands-off approach is still unclear, as long term studies are inconclusive.
- While INVOcell is advertised as half the cost of regular IVF (around $6500 vs. $13,000), many programs, like ours, already offer the low rates and with outstanding success for those same low-risk patients ($7,500). In this “mini-IVF”, ovaries are stimulated with a higher dose, yielding a greater number of eggs that are then cultured in a state-of-the-art lab environment. This allows the production of extra embryos which can be frozen for use at a later date or for additional children in the future. Overall, this makes mini-IVF a much more cost-effective long-term option.
- The manufacturer of INVOcell advertises pregnancy rates at around 20% per cycle. This makes sense, considering the low number of oocytes generated with minimal stimulation. In other words, if a fertile volunteer was to receive minimal stimulation and undergo artificial insemination of normal sperm (IUI), her natural environment would also yield a pregnancy rate of 20% per month. That is because only 1/3 of eggs are chromosomally normal at age 30, 1/5 at age 35, 1/10 at age 40 and 1/20 at age 45. Nothing in IVF improves egg quality over the natural state. One recent study claims a pregnancy rate of 50% which seems outside the normal range over other published studies. Multiple studies about “minimal stimulation IVF” have yielded pregnancy rates in the 20% range because of the limited number of eggs retrieved.
The only time IVF yields higher pregnancy rates is when it generates more eggs and increases the chance of success that particular month. For example, doing IVF with no stimulation, using the one egg naturally ovulated, would be very disappointing despite this approach being marketed as an ideal option. That is because eggs are not better than IVF in the natural state. So if egg DNA is the same, why spend all the cost on a few eggs? Is it not better to spend an extra $1,000 for the use of an IVF Laboratory and another extra $1,000 in medications to generate more eggs for maximizing the chances of success that month rather than having to repeat another cycle to collect additional eggs that are now a few years older? Most patients in our center are not 30 with perfect eggs and perfect sperm. They are older, often with decreased ovarian reserve and significant egg and sperm quality issues that impair fertilization and require an injection of handpicked sperm in each egg (ICSI). Those that are less than 36, with normal ovarian reserve and normal sperm would do much better choosing a more cost-effective option that maximizes outcome, though slightly more expensive overall.
In conclusion, while INVOcell has a slightly lower cost vs. mini-IVF, this device is questionable when computing the real success rate and the risk of having to do another IVF cycle in the future.